
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Cardiovascular Risk/Epidemiology
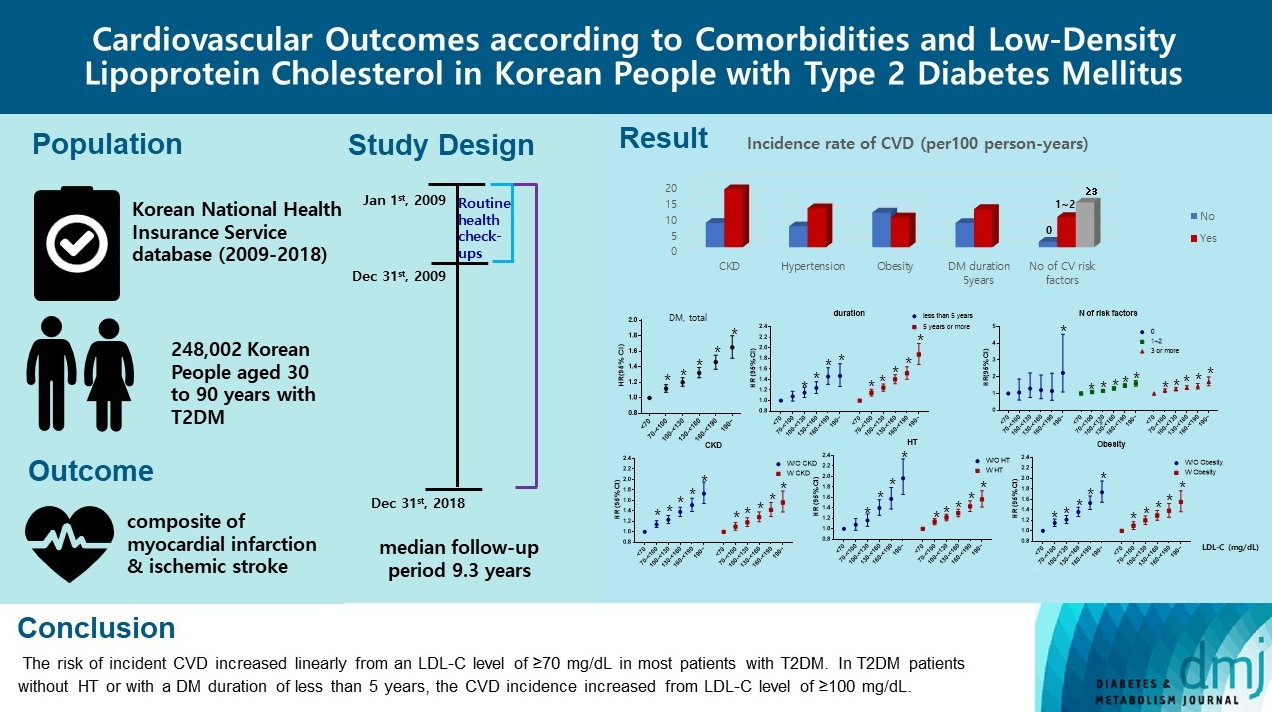
- Cardiovascular Outcomes according to Comorbidities and Low-Density Lipoprotein Cholesterol in Korean People with Type 2 Diabetes Mellitus
- Min Kyong Moon, Junghyun Noh, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong, on Behalf of the Committee of Practice Guideline of Korean Lipid and Atheroscelerosis
- Diabetes Metab J. 2023;47(1):45-58. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0344
- 3,000 View
- 263 Download
- 4 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There are no clear data to support the cardiovascular (CV) risk categories and low-density lipoprotein cholesterol (LDL-C) treatment goals in Korean people with type 2 diabetes mellitus (T2DM). We evaluated the incidence of cardiovascular disease (CVD) according to comorbidities and suggested LDL-C treatment goals in Korean people with T2DM in nationwide cohort data.
Methods
Using the Korean National Health Insurance Service database, 248,002 people aged 30 to 90 years with T2DM who underwent routine health check-ups during 2009 were included. Subjects with previous CVD were excluded from the study. The primary outcome was incident CVD, defined as a composite of myocardial infarction and ischemic stroke during the follow-up period from 2009 to 2018.
Results
The mean age of the study participants was 59.6±10.9 years, and median follow-up period was 9.3 years. CVD incidence increased in the order of DM duration of 5 years or more (12.04/1,000 person-years), hypertension (HT) (12.27/1,000 personyears), three or more CV risk factors (14.10/1,000 person-years), and chronic kidney disease (18.28/1,000 person-years). The risk of incident CVD increased linearly from an LDL-C level of ≥70 mg/dL in most patients with T2DM. In T2DM patients without HT or with a DM duration of less than 5 years, the CVD incidence increased from LDL-C level of ≥100 mg/dL.
Conclusion
For primary prevention of CVD in Korean adults with T2DM, it can be helpful to lower LDL-C targets when there are chronic kidney disease, HT, a long duration of diabetes mellitus, or three or more CV risk factors. -
Citations
Citations to this article as recorded by- Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Optimal Low-Density Lipoprotein Cholesterol Level for Primary Prevention in Koreans with Type 2 Diabetes Mellitus
Ji Yoon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(1): 42. CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Significant Gap Between Guidelines and Practice in the Management of LDL Cholesterol: Insight From the Survey of the Korean Society of Myocardial Infarction
Sang Yeub Lee, Kyung Hoon Cho, Jang Hoon Lee, Young Joon Hong, Jin yong Hwang, Myung Ho Jeong, Weon Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef
- Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
- Cardiovascular Risk/Epidemiology
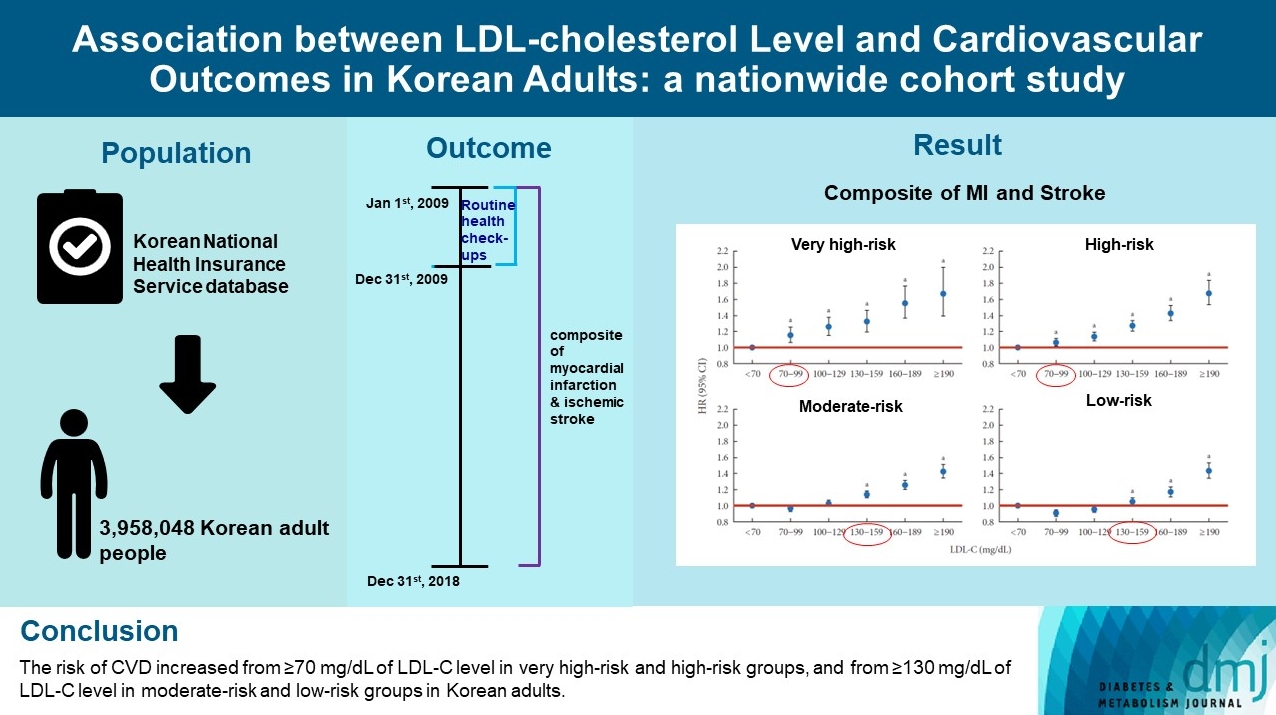
- Association between Low-Density Lipoprotein Cholesterol Level and Cardiovascular Outcomes in Korean Adults: A Nationwide Cohort Study
- Junghyun Noh, Min Kyong Moon, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong, on Behalf of the Committee of Practice Guideline of Korean Lipid and Atheroscelerosis
- Diabetes Metab J. 2023;47(1):59-71. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0320
- 2,770 View
- 225 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To validate the treatment target of low-density lipoprotein cholesterol (LDL-C) level according to the cardiovascular disease (CVD) risk which was recommended by Korean dyslipidemia guideline.
Methods
We used the Korean National Health Insurance Service database which included 3,958,048 people aged 20 to 89 years who underwent regular health screening. The primary outcome was incident CVD, defined as a composite of myocardial infarction and stroke during the follow-up period from 2009 to 2018.
Results
The risk of CVD increased from LDL-C level of 70 mg/dL in very high-risk and high-risk groups and from 130 mg/dL in moderate-risk and low-risk groups. Adjusted hazard ratios (HRs) of LDL-C ranges 70–99, 100–129, 130–159, 160–189, and ≥190 mg/dL were 1.20 (95% confidence interval [CI], 1.08–1.33), 1.27 (1.15–1.42), 1.39 (1.23–1.56), 1.69 (1.45–1.96), and 1.84 (1.49– 2.27) in very high-risk group, and 1.07 (1.02–1.13), 1.16 (1.10–1.21), 1.29 (1.22–1.36), 1.45 (1.36–1.55), and 1.73 (1.58–1.90) in high-risk group. Adjusted HRs (95% CI) of LDL-C ranges 130–159, 160–189, and ≥190 mg/dL were 1.15 (1.11–1.20), 1.28 (1.22– 1.34), and 1.45 (1.36–1.54) in moderate-risk group and 1.07 (1.02–1.13), 1.20 (1.13–1.26), and 1.47 (1.37–1.57) in low-risk group.
Conclusion
We confirmed the incidence of CVD was increased in higher LDL-C range. The risk of CVD increased from ≥70 mg/dL of LDL-C in very high-risk and high-risk groups, and from ≥130 mg/dL of LDL-C in moderate-risk and low-risk groups in Korean adults. -
Citations
Citations to this article as recorded by- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
Byung Jin Kim, Kwang Soo Cha, Wook Hyun Cho, Eung Ju Kim, Seung-Hyuk Choi, Moo Hyun Kim, Sang-Hyun Kim, Jun-Bean Park, Seong-Mi Park, Il Suk Sohn, Kyu Hyung Ryu, In-Ho Chae
Journal of Cardiovascular Pharmacology and Therapeutics.2023;[Epub] CrossRef
- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
- Response: Association between Cigarette Smoking and New-Onset Diabetes Mellitus in 78,212 Koreans Using Self-Reported Questionnaire and Urine Cotinine (
Diabetes Metab J 2020;44:426–35) - Ji Hye Kim, Byung Jin Kim
- Diabetes Metab J. 2020;44(4):623-624. Published online August 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0169
- [Original]
- 4,201 View
- 67 Download
- Metabolic Risk/Epidemiology
- Association between Cigarette Smoking and New-Onset Diabetes Mellitus in 78,212 Koreans Using Self-Reported Questionnaire and Urine Cotinine
- Ji Hye Kim, Dae Chul Seo, Byung Jin Kim, Jeong Gyu Kang, Seung Jae Lee, Sung Ho Lee, Bum Soo Kim, Jin Ho Kang
- Diabetes Metab J. 2020;44(3):426-435. Published online November 1, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0068
- 6,681 View
- 94 Download
- 13 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background No study has assessed association between cigarette smoking and new-onset diabetes mellitus (NODM) incidence using two different smoking classification systems: self-reported questionnaire and urine cotinine. The objective of this longitudinal study was to evaluate NODM risk using the above two systems in Korean adults.
Methods Among individuals enrolled in Kangbuk Samsung Health Study and Cohort Study who visited between 2011 and 2012 at baseline and 2014 at follow-up, 78,212 participants without baseline diabetes mellitus were followed up for a median of 27 months. Assessment of NODM incidence was made at the end of follow-up period. Cotinine-verified current smoking was having urinary cotinine ≥50 ng/mL.
Results Percentages of self-reported and cotinine-verified current smokers were 25.9% and 23.5%, respectively. Overall incidence of NODM was 1.5%. According to multivariate regression analyses, baseline self-reported current smoking (relative risk [RR], 1.33; 95% confidence interval [CI], 1.07 to 1.65) and cotinine-verified current smoking (RR, 1.27; 95% CI, 1.08 to 1.49) increased NODM risk compared to baseline self-reported never smoking and cotinine-verified current non-smoking. Higher daily amount and longer duration of smoking were also associated with increased NODM risk (
P for trends <0.05). In particular, self-reported current smokers who smoked ≥20 cigarettes/day (RR, 1.62; 95% CI, 1.25 to 2.15) and ≥10 years (RR, 1.34; 95% CI, 1.08 to 1.67) had the highest RRs for NODM. These results remained significant in males, although there was no gender interaction.Conclusion This longitudinal study showed that baseline self-reported and cotinine-verified current smoking were associated with increased risks of NODM, especially in males.
-
Citations
Citations to this article as recorded by- Variability in the association of smoking status with the prevalence of diabetes mellitus in the Korean population according to different definitions of smoking status: analysis based on the Korea National Health and Nutrition Examination Survey (2014-202
Yechan Kyung, Young Sook Park, Mi Hyeon Jin, Hae Jeong Lee
International Journal of Environmental Health Research.2024; : 1. CrossRef - Determination of Diabetes-associated Cardiovascular Autonomic Neuropathy Risk Factors among Insulin and Non-insulin Dependent Diabetics
Ibrahim Abdulsada, Zain Alabdeen Obaid, Farah Almerza, Mays Alwaeli, Anmar Al-Elayawi, Taha Al-Dayyeni, Harir Al-Tuhafy
The Journal of Medical Research.2023; 9(6): 141. CrossRef - Trends and Risk Factors of Metabolic Syndrome among Korean Adolescents, 2007 to 2018 (Diabetes Metab J 2021;45:880-9)
Jiun Chae, Moon Young Seo, Shin-Hye Kim, Mi Jung Park
Diabetes & Metabolism Journal.2022; 46(2): 351. CrossRef - Xenobiotics Delivered by Electronic Nicotine Delivery Systems: Potential Cellular and Molecular Mechanisms on the Pathogenesis of Chronic Kidney Disease
Pablo Scharf, Felipe Rizzetto, Luana Filippi Xavier, Sandra Helena Poliselli Farsky
International Journal of Molecular Sciences.2022; 23(18): 10293. CrossRef - Cigarette Smoking Increases the Risk of Type 2 Diabetes Mellitus in
Patients with Non-Alcoholic Fatty Liver Disease: A Population-Based Cohort
Study
Chan Liu, Yanqin Wu, Wenjuan Duan, Wenming Xu
Experimental and Clinical Endocrinology & Diabetes.2022; 130(12): 793. CrossRef - Current status of health promotion in Korea
Soo Young Kim
Journal of the Korean Medical Association.2022; 65(12): 776. CrossRef - Association between secondhand smoke exposure and diabetes mellitus in 131 724 Korean never smokers using self‐reported questionnaires and cotinine levels: Gender differences
Byung Jin Kim, Ji Hye Kim, Jeong Gyu Kang, Bum Soo Kim, Jin Ho Kang
Journal of Diabetes.2021; 13(1): 43. CrossRef - Changes in creatinine‐to‐cystatin C ratio over 4 years, risk of diabetes, and cardiometabolic control: The China Health and Retirement Longitudinal Study
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Journal of Diabetes.2021; 13(12): 1025. CrossRef - Trends in the Socioeconomic Inequalities Related to Second-Hand Smoke Exposure as Verified by Urine Cotinine Levels Among Nonsmoking Adults: Korea National Health and Nutrition Examination Survey 2008–2018
Seo Young Kang, Min Kyung Lim, Hong-Jun Cho
Nicotine & Tobacco Research.2021; 23(9): 1518. CrossRef - Letter: Association between Cigarette Smoking and New-Onset Diabetes Mellitus in 78,212 Koreans Using Self-Reported Questionnaire and Urine Cotinine (Diabetes Metab J 2020;44:426–35)
Bo-Yeon Kim
Diabetes & Metabolism Journal.2020; 44(4): 619. CrossRef - Response: Association between Cigarette Smoking and New-Onset Diabetes Mellitus in 78,212 Koreans Using Self-Reported Questionnaire and Urine Cotinine (Diabetes Metab J 2020;44:426–35)
Ji Hye Kim, Byung Jin Kim
Diabetes & Metabolism Journal.2020; 44(4): 623. CrossRef - Smoking as a Target for Prevention of Diabetes
Ye Seul Yang, Tae Seo Sohn
Diabetes & Metabolism Journal.2020; 44(3): 402. CrossRef
- Variability in the association of smoking status with the prevalence of diabetes mellitus in the Korean population according to different definitions of smoking status: analysis based on the Korea National Health and Nutrition Examination Survey (2014-202
- The Relationship between Serum Retinol-Binding Protein 4 Levels and Coronary Artery Disease in Korean Adults.
- Ji Hoon Kim, Eun Jung Rhee, Eun Suk Choi, Jong Chul Won, Cheol Young Park, Won Young Lee, Ki Won Oh, Byung Jin Kim, Ki Chul Sung, Bum Soo Kim, Jin Ho Kang, Sung Woo Park, Sun Woo Kim, Man Ho Lee, Jung Roe Park
- Korean Diabetes J. 2009;33(2):105-112. Published online April 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.2.105
- 7,743 View
- 16 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
A recently discovered adipokine, retinol-binding protein-4 (RBP-4), is reportedly associated with insulin resistance and metabolic syndrome. This study was performed to analyze the relationship between serum RBP-4 levels and coronary artery disease (CAD) in Korean adults. METHODS: In 235 subjects (mean age 58 years) in whom coronary artery angiograms were performed due to complaints of chest pain, serum RBP-4 levels were measured by enzyme-linked immunosorbent assay. Coronary artery angiograms were performed in all subjects and the severity of CAD was assessed by the number of stenotic vessels. The presence of metabolic syndrome was defined by AHA/NHLBI criteria with body mass index substituted for waist circumference. RESULTS: Coronary angiogram showed that 101 subjects (43%) had normal coronary vessel, 82 subjects (34.9%) had 1-vessel disease, 31 subjects (13.2%) had 2-vessel disease and 21 subjects (8.9%) had 3-vessel disease. Subjects with coronary artery stenosis showed a higher mean age (60.5 +/- 10.0 years), fasting glucose (123.3 mg +/- 45.0 mg/dL) and lower mean value for high-density lipoprotein cholesterol (HDL-C) level (49.0 +/- 13.2 mg/dL), although serum RBP-4 levels were not significantly different between those with and without CAD. Mean age and fasting glucose level increased significantly as the number of stenotic vessels increased, although serum RBP4 level showed no significant differences among the different groups. Among the metabolic parameters, only serum triglyceride levels showed a significant correlation with serum RBP-4 levels. CONCLUSION: There was no difference in mean serum RBP-4 levels between subjects with or without coronary artery disease in Korean adults. Further studies are warranted to draw a clear conclusion on the effect of RBP-4 on atherosclerosis. -
Citations
Citations to this article as recorded by- Retinol binding protein 4 levels relate to the presence and severity of coronary artery disease
Gokay Nar, Sara Sanlialp, Rukiye Nar
Journal of Medical Biochemistry.2021; 40(4): 384. CrossRef
- Retinol binding protein 4 levels relate to the presence and severity of coronary artery disease
- The Association of Pro12Ala Polymorphism in PPAR-gamma Gene with Coronary Artery Disease in Korean Subjects.
- Chang Hee Kwon, Eun Jung Rhee, Se Yeon Kim, Eun Ran Kim, Chang Uk Chon, Chan Hee Jung, Ji Ho Yun, Byung Jin Kim, Ki Chul Sung, Bum Su Kim, Won Young Lee, Ki Won Oh, Jin Ho Kang, Sun Woo Kim, Man Ho Lee, Jung Roe Park
- Korean Diabetes J. 2006;30(2):122-129. Published online March 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.2.122
- 2,282 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
PPAR-gamma, a member of nuclear family, which is involved in the differentiation of adipose tissue, is reported to be associated in the pathogenesis of type 2 diabetes mellitus, insulin resistance and atherosclerosis. We conducted a research to see whether the prevalence of coronary artery disease is associated with Pro12Ala polymorphism in exon B of PPAR-gamma in Korean adults. METHODS: The study was conducted in 161 subjects (97 males, 64 females, mean age 57 year old) who underwent coronary angiogram due to chest pain. We assessed cardiovascular risk factors in all subjects, such as blood pressure, body mass index (BMI), fasting blood sugar and serum lipid profiles. Subjects were divided into four groups as normal, 1-vessel, 2-vessel and 3-vessel disease according to the number of stenosed coronary arteries. Genotypings of Pro12Ala polymorphism were done with Real-time polymerase chain reaction. RESULTS: Allelic frequency for proline was 0.957 and 0.043 for alanine, and they were in compliance with Hardy-Weinberg equilibrium (P = 0.85). 79 subjects (43.5%) had normal coronary artery, 52 subjects (31%), 1-vessel disease, 24 subjects (14.9%), 2-vessel disease and 15 subjects (9.3%), 3-vessel disease. When the cardiovascular risk factors were compared among these four groups, there were no meaningful differences except the age and high-density lipoprotein cholesterol levels, which were lost after adjustment for age and BMI. There were no significant differences in the prevalence or severity of coronary artery diseases according to the different genotypes of Pro12Ala polymorphism. CONCLUSIONS: There was no significantassociation between Pro12Ala polymorphism in exon B of PPAR-gamma and prevalence or severity of coronary artery disease in Korean adults. It is considered that further studies on the correlation between Pro12Ala polymorphism and coronary artery disease should be carried out in larger Korean population in the future

 KDA
KDA
 First
First Prev
Prev





